Attention Deficit Hyperactivity Disorder (ADHD) is a prevalent neurodevelopmental disorder in children and adolescents, significantly impacting cognitive learning and social interactions. Methylphenidate (MPH) is the primary pharmacological treatment for ADHD; however, parents’ concerns about potential side effects, including self-harm and suicide, have posed substantial challenges for clinical management. Professor Tzu-Chi Lee from the Department of Health Promotion and Health Education at National Taiwan Normal University has pioneered research in Taiwan to clarify the relationship between MPH use and mortality rates. The findings reveal that individuals who use MPH exhibit lower overall mortality rates compared to those who do not. Additionally, earlier initiation of MPH treatment following an ADHD diagnosis, as well as long-term use of the medication, is associated with further reductions in mortality risk.
Professor Tzu-Chi Lee specializes in biostatistics and big data analysis, leveraging extensive datasets from health and medical databases to provide novel insights for clinical medicine. Using high-efficiency analytical programs he developed himself, and employing methods from epidemiology and genomics, his work frequently sheds light on complex medical phenomena. His research topics often stem from "unexplained cases" encountered by pediatric psychiatrists during clinical practice—issues that lack clear scientific explanations. Resolving these challenges typically requires his expertise in statistical research to provide empirical evidence and support.
Over the past two decades, methylphenidate (MPH) has been regarded as the primary medication for ADHD treatment. Professor Lee noted that some physicians have reported parental concerns regarding side effects observed in their children after taking the medication. However, these concerns are not centered on the commonly listed side effects, such as sleep disturbances or appetite loss, as indicated on the package insert. Instead, parents are particularly worried about anecdotal cases they have heard of, such as incidents of suicide or accidents occurring after medication use. The lack of causal research on such cases has contributed to parents viewing MPH use with apprehension. This skepticism often leads to medication discontinuation or interruption, significantly impacting the effectiveness of treatment.
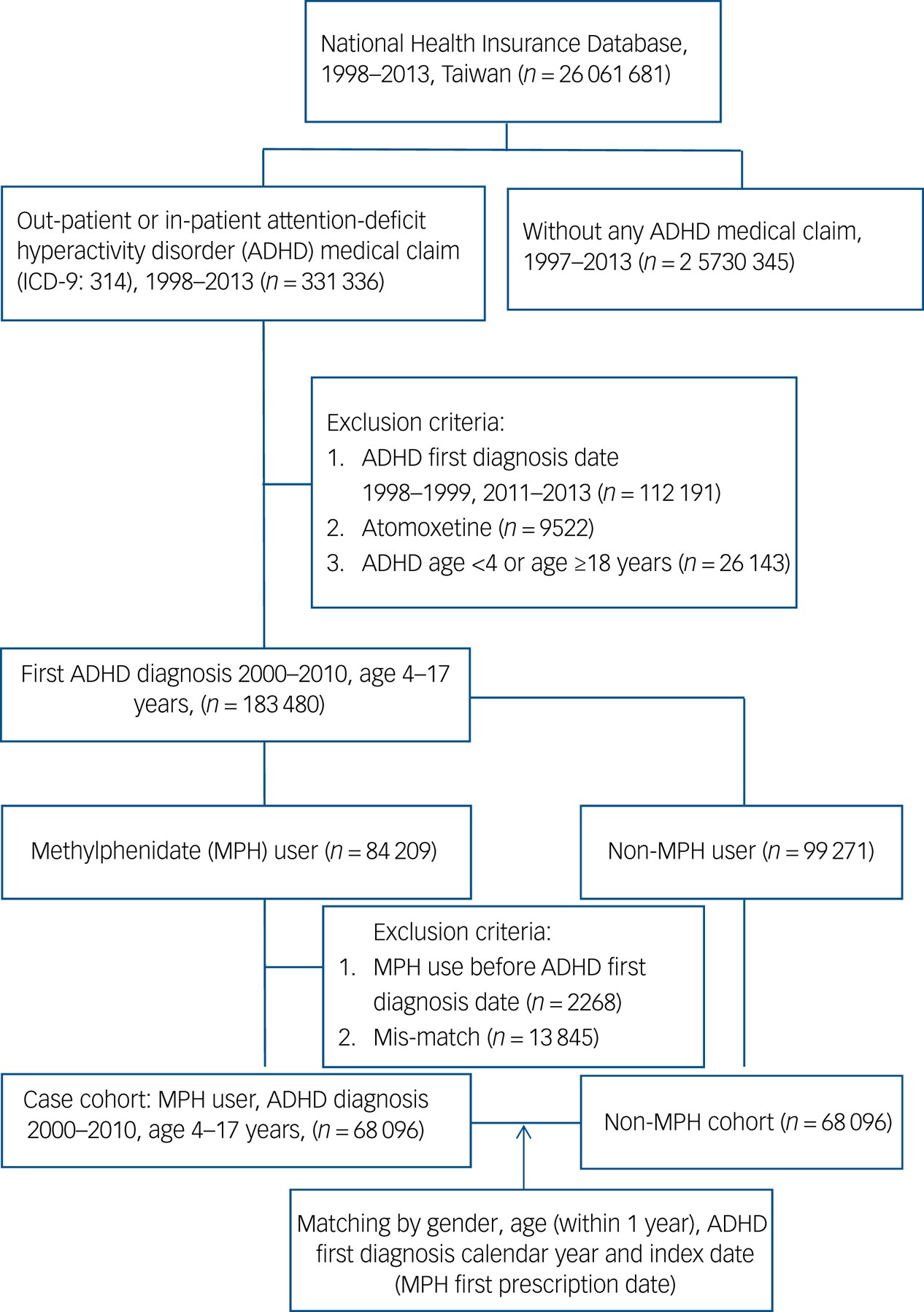
In response to clinical physicians' requests for assistance, Professor Lee embarked on a comprehensive study, revisiting and adopting a novel research methodology to conduct a "repeated measures cohort study." At the outset, he accessed Taiwan's National Health Insurance Research Database (NHIRD) through the Ministry of Health and Welfare, identifying a cohort of 68,096 children and adolescents aged 4 to 17 who had been diagnosed with ADHD and prescribed MPH between the years 2000 and 2010. He analyzed the annual dosage of MPH prescribed, and employed a Cox regression model with repeated measures to examine the association between MPH use and mortality rates.
Professor Lee further categorized mortality into natural causes (e.g., physical illness) and non-natural causes (e.g., suicide, accidents, homicide). The study revealed that MPH use did not increase mortality from natural causes. More notably, the mortality rate from non-natural causes during periods of MPH use was lower than during periods without MPH use. This analysis confirmed that MPH not only does not contribute to deaths from natural causes, but also provides a protective effect against non-natural causes of mortality.
A 2020 epidemiological study on ADHD in Taiwan reported that 8.7% of school-aged children and adolescents met the diagnostic criteria for ADHD, equating to approximately 220,000 individuals. However, when compared with statistical data from the National Health Insurance database, the prevalence rate of ADHD was only 2.44%, indicating that most children have not received proper diagnosis and treatment. This disparity is likely influenced by the stigma surrounding the disorder, as well as parental attributions of symptoms to personality traits or school disciplinary methods. Without consistent treatment, an estimated 60% of individuals with ADHD will continue to experience symptoms into adulthood.
The findings of this study underscore the critical importance of early detection and treatment in influencing the progression of ADHD. In addition to examining the relationship between MPH use and mortality, Professor Lee further analyzed the differences between early, long-term use and late, short-term use of the medication. The results revealed that patients who began MPH treatment earlier and adhered to long-term usage exhibited significantly lower mortality rates. In other words, when parents observe temporary symptom relief in their children and request discontinuation of medication, physicians may use this research to support the recommendation for continued treatment and advise parents that long-term use may yield greater benefits.
This study not only provides safety guidance for ADHD patients using MPH, but also offers clinical physicians robust data support. However, the research data span from 2000 to 2013, and with the rapid advancement of pharmacological developments, new ADHD medications have emerged in recent years. Future research could extend to analyzing MPH usage data from 2014 to 2024, as well as evaluating the efficacy of alternative treatments. Additionally, investigations into the comparative effectiveness of single-drug versus combination therapies could offer further insights into optimizing ADHD treatment.
Figure 1: Data selection flowchart of this study
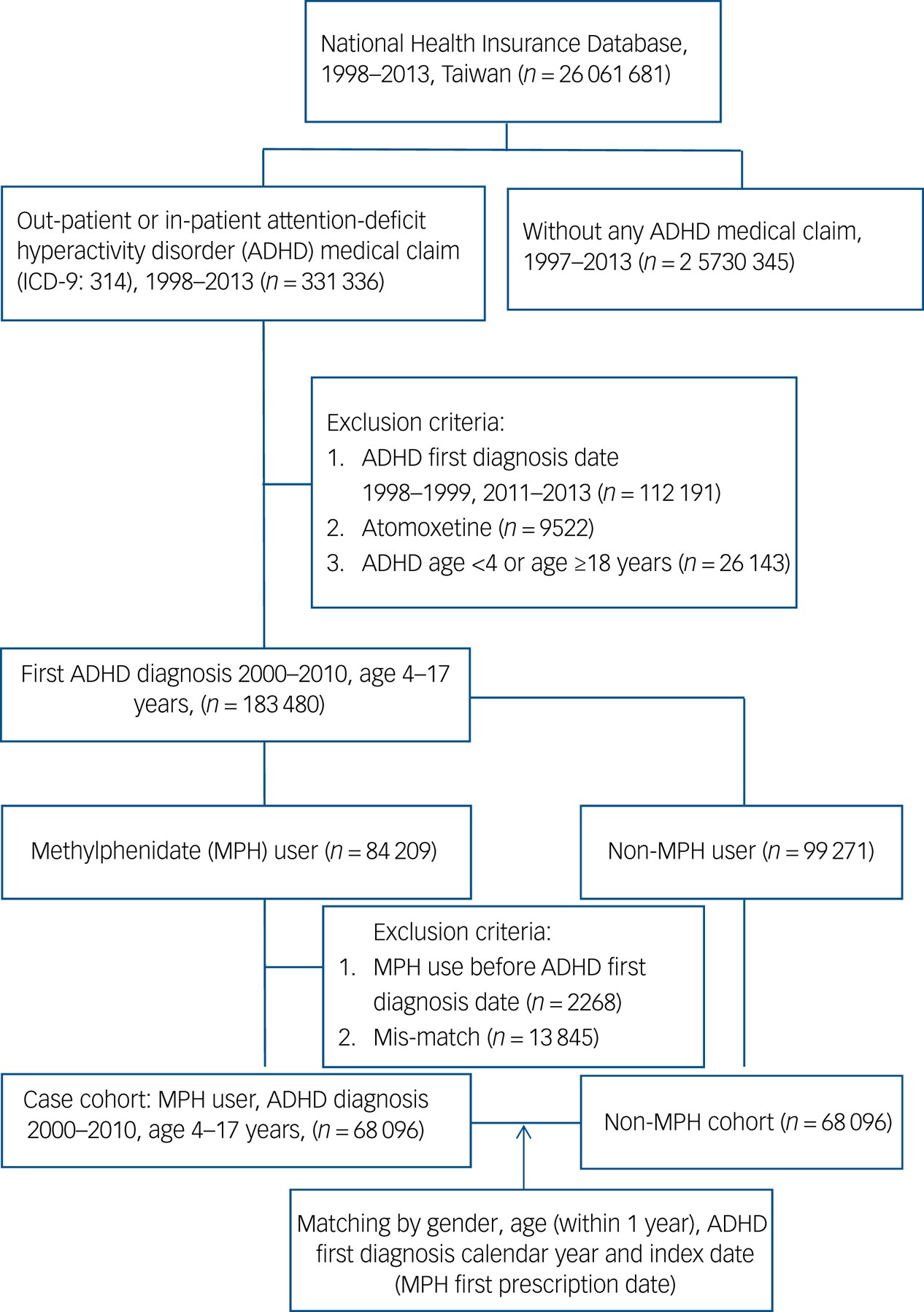
This study utilized data from Taiwan's National Health Insurance Research Database, focusing on 183,480 children and adolescents aged 4 to 17 newly diagnosed with ADHD (International Classification of Diseases, Ninth Revision (ICD-9): 314) between 2000 and 2010. This age group was chosen because ADHD is rarely diagnosed outside this range. The primary objective of the analysis was to examine the relationship between MPH treatment and mortality rates.
Between 2000 and 2010, MPH was the primary medication used for treating ADHD in Taiwan. Atomoxetine was approved for use in Taiwan in 2007; however, its prescription rate was much lower than that of MPH, accounting for only 4% of all ADHD patients. As a result, this study excluded participants who were prescribed Atomoxetine.
To better control for the influences of gender, birth year, and the year of initial ADHD diagnosis, the research team used exact matching to select a control group of 68,096 children and adolescents who were not prescribed MPH, but matched the MPH group in terms of gender, birth year, and ADHD diagnosis year. Both groups were followed from the study baseline (the date of the first MPH prescription) until death, migration, or the end of the observation period on December 31, 2013. The flowchart systematically illustrates the process of exclusion and selection of study participants, establishing two comparable study groups—those who used MPH and those who did not—balanced in terms of gender, birth year, and ADHD diagnosis year, for subsequent analysis. (This article was provided by The Center of Public Affairs.)
Source: Chen, V. C. H., Chan, H. L., Wu, S. I., Lu, M. L., Dewey, M. E., Stewart, R., & Lee, C. T. C. (2022). Methylphenidate and mortality in children with attention-deficit hyperactivity disorder: Population-based cohort study.
British Journal of Psychiatry, 220(2), 64-72.
https://doi.org/10.1192/bjp.2020.129